Claim Submission Guidelines
Health and Dental Claims
How to Submit Claims...
| RWAM Plan Member Services Website |
| Claims can be submitted online by signing in to the Plan Member Services website.
|
| RWAM Mobile App |
| You can enjoy the on-the-go convenience of the RWAM Mobile App, once you have registered for Plan Member Services. Submitting a claim with the RWAM Mobile App is as simple as taking a picture of your receipt and answering a few questions. |
| Paper Form |
| Submitting a claim using the traditional paper form still works.
|
| Provider Direct Submission |
| Once you have registered for Plan Member Services, you can ask your Healthcare Provider to submit your claims to RWAM for immediate adjudication and information regarding the eligibility of your claim. Eligible reimbursement may be made directly to your bank account or payment can be made to your Provider. For more information on Provider submission of claims visit our Provider eServices page and Provider FAQs page. |
Are you covered by more than one benefit plan?
Coordinate between multiple plans to maximize your coverage. Review the Coordination of Benefits page and receive up to 100% coverage for eligible expenses.
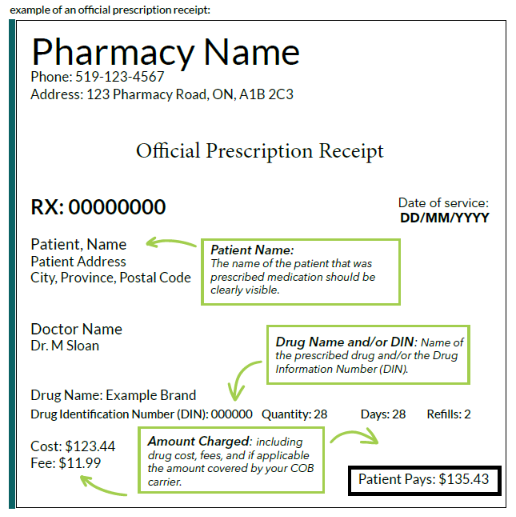
Drug Claim Submission Requirements
Submitting Your Prescription Claim With RWAM Is Easy!
To submit your claim, you will need to scan or take a picture of your official prescription receipt ensuring all information is clearly visible and there are no shadows, markings or obstructions. Use the RWAM Plan Member Services website or RWAM Mobile App to submit your claim, attach the photo or scanned copy of the official prescription receipt, and click “Submit”. It’s that easy!
For prescription drug claim submissions, RWAM will require an official prescription receipt - often you will find it attached or inside your prescription takeaway package you receive from the pharmacy.
Receipt MUST Include:
Patient Name - The name of the patient that was prescribed and will use the medication must be clearly visible.
Drug Name and/or DIN - The name of the prescribed drug and/or the Drug Information Number (DIN) must be clearly visible.
Amount Charged - The total cost including drug cost, fees, and if applicable the amount covered by your drug plan must be clearly visible.
Download the Informational PDF "Drug Claim Submission Requirements"
Did you know?
For most extended health, dental and drug claims, active plan members can submit their claim up to 12 months from the date of occurrence, regardless of year end of calendar date. Download the Informational PDF "Claim Submission Deadlines" to learn more!
All Other Claims
| Claim Type | How to Submit Claims |
| Travel Assist | For Out-of-Province / Out-of-Canada (OOC) Claims complete the Travel Assist Out-of-Canada / Out-of-Province Claim Form. |
| Critical Illness | Contact your Plan Administrator or Contact Us for Critical Illness claims assistance. |
| Disability | Appropriate claim forms based on your group's coverage are available from your Plan Administrator or Contact Us. |
| Life Insurance or Accidental Death & Dismemberment | Contact Us and ask for Life claims assistance. |
Have questions about submitting your Claim?
- Read the fact sheet "Extended Health Care Benefits - What's covered?" to learn how to determine whether your Group Health Benefits Plan includes coverage for a particular provider.
- Review the "Understanding Your Group Insurance Benefits" fact sheet to learn how certain rules, limits, and maximums which govern how much of your claim is eligible for reimbursement are applied to each and every claim.
- Check out the Claims FAQs for Plan Members for answers to common claim questions.
- Need more information? Please Contact Us.
Patient Choice Cards
In cases where your group plan doesn't cover the full cost, Patient Choice Cards may allow you to access your preferred brand name medications with a minimum of out-of-pocket expense .
Registration is FREE, and you can register for multiple programs in order to access the brand name product(s) you wish to receive. To learn more about either program and to view a current list of the medications covered by each, please visit the www.RxHelpONE.com and www.innovicares.ca websites.
Note the content of these programs may change, and coverage for specific brands can be discontinued at any time. RWAM provides this information on the free RxHelp ONETMand innoviCares patient choice card programs as an option for Plan Members. This is not an endorsement.
Connect With Us
Call Us 1-877-888-7926 or Email Us
Our team is here to help. Discover the RWAM advantage.